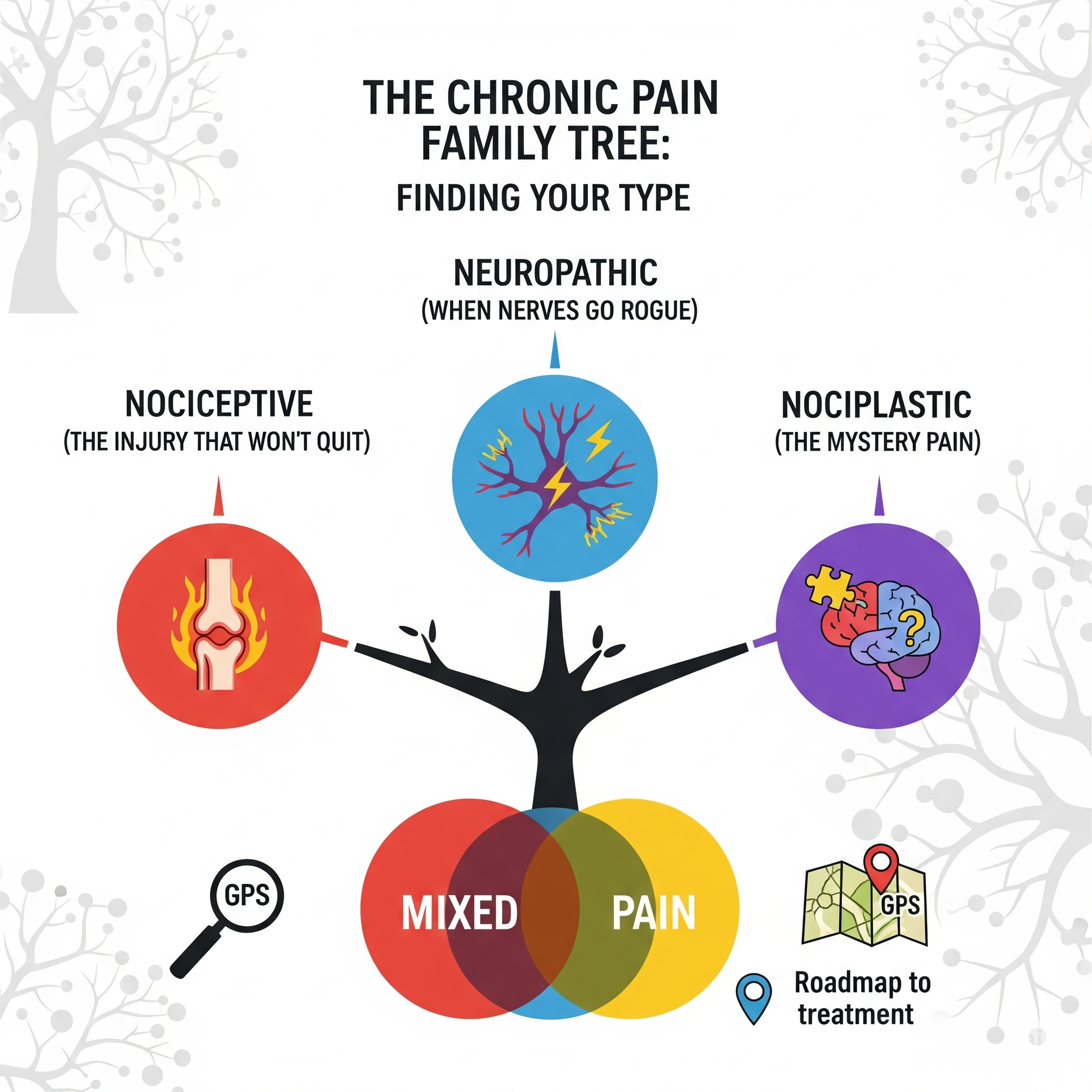
There are Different Types of Chronic Pain : Which one is yours?
Not all chronic pain is created equal—and knowing your type changes everything about your approach.
Here's something that might blow your mind: There are actually three completely different types of chronic pain.They look similar from the outside (they all hurt), but they're as different as a broken bone, a rash, and a migraine.
And here's why this matters: The treatment that works amazingly for one type might be completely useless—or even harmful—for another.
It's like trying to fix a leaky faucet with a band-aid, or treating a sunburn with cough medicine. You're not going to get very far if you're using the wrong approach for your specific problem.
🎯 Why These Labels Actually Matter (And It's Not Just Medical Jargon)
I get it. More medical terms, more categories—sometimes it feels like doctors just love making things complicated. But stick with me here, because understanding your pain type is like having a GPS for your treatment journey.
🗺️ When you know your type, you can:
Ask for treatments that actually work for YOUR kind of pain
Avoid wasting time (and money) on approaches that won't help
Advocate for yourself when doctors suggest treatments that don't make sense for your condition
Connect with others who have the same type of pain (because their strategies might actually work for you)
Think of it like this: if you walked into a pharmacy and just asked for "medicine," they'd look at you like you'd lost your mind. Medicine for what? A headache? High blood pressure? An infection? Pain works the same way—the more specific you can be, the better help you can get.
👪 The Big Three: Meet The Chronic Pain Family
—
🔥 Type 1: Nociceptive Pain - "The Injury That Won't Quit"
What it is: This is pain from actual tissue damage or inflammation that either won't heal or keeps getting re-injured. Your pain alarm system is working correctly—there's just ongoing damage to report.
💭 What it feels like: Usually aching, throbbing, or sharp. It often gets worse with movement and better with rest. The pain makes sense with what you're doing.
📝 Common examples:
Arthritis (your joints are actually inflamed)
Cancer pain (tumors pressing on tissues)
Chronic back pain from disc problems
Ongoing injury that won't heal properly
✨ The silver lining: This type often responds well to traditional pain treatments because there's something concrete to target.
🎯 What this means for your treatment:
✅ Anti-inflammatory medications might actually help
✅ Physical therapy focusing on the problem area makes sense
✅ Heat, cold, and topical treatments can be effective
✅ Sometimes procedures that target the specific problem area work well
⚡ Type 2: Neuropathic Pain - "When Nerves Go Rogue"
What it is: Your nerves themselves are damaged or misbehaving. It's like having faulty electrical wiring that keeps sending "FIRE!" signals to your brain when there's no fire.
💭 What it feels like: Often described as burning, electric, shooting, or tingling. It might feel like pins and needles, or like someone's running electrical current through your body. Sometimes even light touch feels awful.
📝 Common examples:
Diabetic neuropathy (high blood sugar damages nerves)
Sciatica (compressed nerve in your back)
Post-shingles pain
Some types of chronic headaches
🔄 The plot twist: Regular pain medications often don't work well for this type. But medications originally designed for seizures or depression? They can be game-changers¹.
🎯 What this means for your treatment:
✅ Nerve-specific medications (like gabapentin, pregabalin) might be more helpful than traditional painkillers
✅ Treatments that target nerve function (like certain physical therapy techniques) can be effective
✅ Sometimes procedures that block or reset nerve signals work better than those targeting tissues
✅ Heat might help, but sometimes cold works better (it varies by person)
🔍 Type 3: Nociplastic Pain - "The Mystery Pain"
What it is: Your pain processing system has become hypersensitive, but there's no clear tissue damage or nerve problem. Your pain is 100% real, but doctors scratch their heads at your normal test results.
💭 What it feels like: Often widespread, can change locations, might be described as deep aching, burning, or just "everything hurts." It's often accompanied by fatigue, sleep problems, and brain fog.
📝 Common examples:
Fibromyalgia
Some chronic headaches
Irritable bowel syndrome pain
Some cases of chronic fatigue syndrome
😤 The frustrating part: This is the type that often leaves people feeling gaslit by the medical system because "everything looks normal" on tests.
🎯 What this means for your treatment:
✅ Focus on treatments that calm down your oversensitive nervous system
✅ Sleep improvement is crucial (poor sleep makes this type much worse)
✅ Stress management isn't just helpful—it's essential
✅ Gentle, gradual exercise can help retrain your nervous system
✅ Some antidepressants work well (not because you're depressed, but because they affect pain processing)²
🎭 When Life Gives You a Combo Deal: Mixed Pain
🌪️ Plot twist: Many people don't fit neatly into just one category. You might have:
Arthritis in your knee (nociceptive)
That's also pinching a nerve (neuropathic)
And the chronic stress of dealing with both has made your whole system hypersensitive (nociplastic)
This is actually really common. It's like having multiple apps running on your phone at once—they all affect each other and drain your battery faster.
🎯 What this means: Your treatment plan might need to address multiple types of pain simultaneously. This is why cookie-cutter approaches often don't work for chronic pain.
🕵️♀️ Your Pain Detective Kit: Simple Questions to Figure Out Your Type
Ask yourself:
🔍 Does your pain match up with something specific that's wrong? (Joint damage, known injury, etc.) → Likely nociceptive component
⚡ Does it feel electric, burning, or shooting? Does light touch make it worse? → Possible neuropathic component
🌐 Is your pain widespread and hard to pinpoint? Do you also have fatigue, sleep issues, or brain fog? → Possible nociplastic component
📍 Does your pain move around or change characteristics? → Often suggests nociplastic involvement
💊 Do traditional painkillers barely touch it? → More likely neuropathic or nociplastic
Remember: These questions are just starting points. Only a healthcare provider who understands chronic pain can make an official determination.
💬 Questions to Ask Your Doctor (So You Get Answers That Actually Help)
❌ Instead of: "Why do I hurt?" ✅ Try: "Based on my symptoms, which type of chronic pain mechanism do you think is most likely—nociceptive, neuropathic, or nociplastic?"
❌ Instead of: "What can you give me for pain?" ✅ Try: "Given my pain type, what treatments have the best evidence for effectiveness?"
❌ Instead of: "How long will this last?" ✅ Try: "What would successful management look like for my specific type of pain?"
🚨 Red Flags: When to Seek Help Immediately
📞 Call for emergency help if you experience:
Sudden, severe pain that's completely different from your usual pain
Pain with fever, especially if you have any implants or recent procedures
Pain with weakness, numbness, or loss of bladder/bowel control
Severe headache with vision changes, confusion, or stiff neck
Chest pain or pain that radiates to your jaw, arm, or back
🏥 See your doctor soon if:
Your usual pain pattern changes significantly
New symptoms develop alongside your pain
Your current treatments stop working suddenly
You develop new areas of pain
🎯 The Bottom Line: Knowledge Really Is Power
Understanding your pain type isn't about getting a fancy diagnosis to impress people at parties. It's about finally having a roadmap that makes sense for your specific situation.
Once you know whether you're dealing with tissue damage, nerve problems, or a hypersensitive system (or some combination), you can stop wasting time on treatments that were never going to work for your type of pain.
Your next step: Take a honest look at your pain using the detective questions above. Then, have a conversation with a healthcare provider who understands chronic pain. Come prepared with your observations and specific questions about treatment approaches for your likely pain type.
Remember: You deserve treatments that are designed for the type of pain you actually have, not just generic "pain management”.
Want to track your pain patterns to help identify your type?
Download our free "Pain Pattern Tracker" to gather the information that will help you and your healthcare team determine the best approach for YOUR pain
📚 References:
Finnerup, N.B., et al. (2015). "Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis." The Lancet Neurology, 14(2), 162-173.
Clauw, D.J. (2014). "Fibromyalgia: a clinical review." JAMA, 311(15), 1547-1555.
Kosek, E., et al. (2016). "Do we need a third mechanistic descriptor for chronic pain states?" Pain, 157(7), 1382-1386.