Understanding central sensitization: Why your pain system gets stuck on "high alert"
You wake up and your sheets hurt.
Not uncomfortable—they actually hurt. The soft cotton feels like sandpaper on your skin.
You get out of bed and every step hurts your legs, even though you didn't injure anything. Your partner hugs you and you pull away because it hurts like a huge bruise.
Sound familiar?
Maybe for you it's different. Maybe it's headaches that started after a car accident. The doctors say you healed, but the pain never left. Or back pain that started in one place but now spreads everywhere. Or a diagnosis that took five doctors and three years to get.
Here's what's happening: your pain system has been rewired.
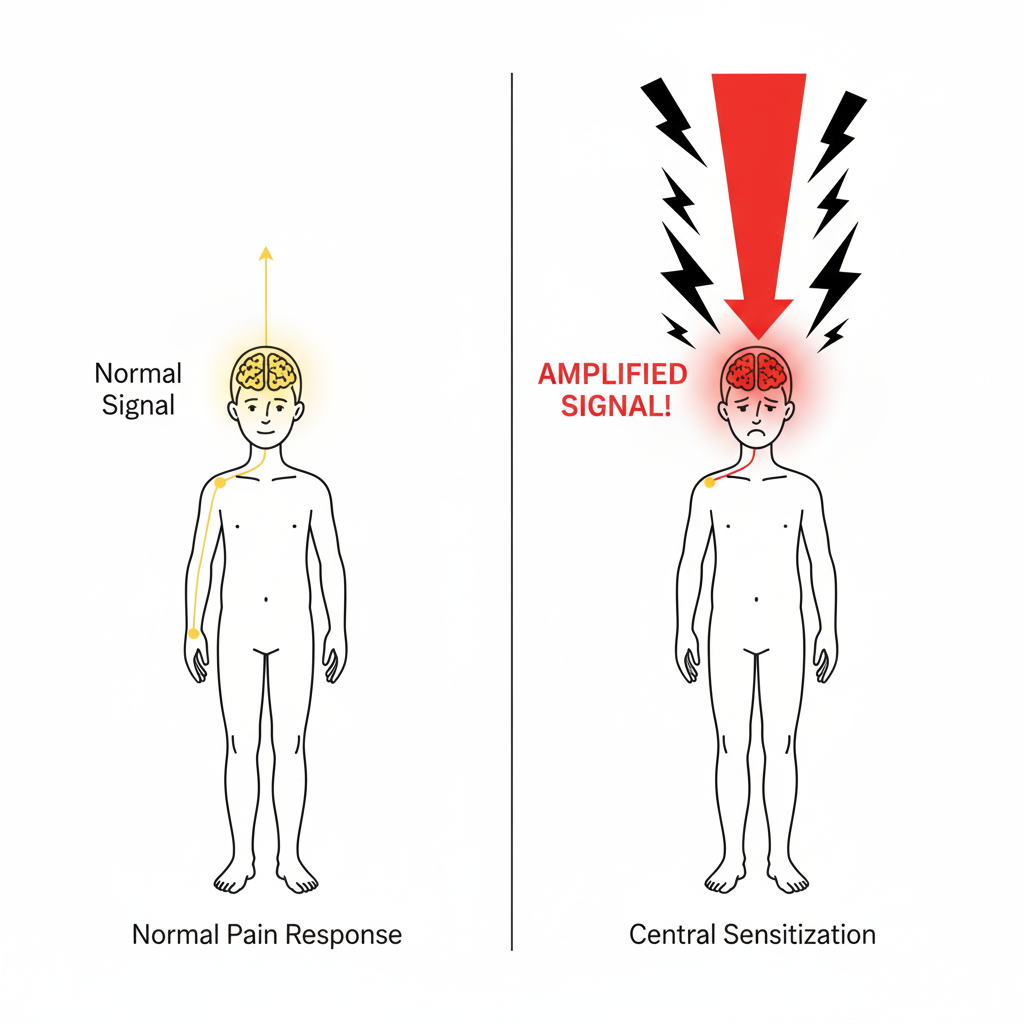
Central sensitization means your nervous system has become too sensitive over time. Your brain and spinal cord amplify danger signals even when there's no real threat that damage your body.
In this article, you'll learn:
What central sensitization is
How to know if you have it
Why it happens
How to treat it
There is no visible lesion, but yet, your pain is real. The changes in your nervous system are real. And you can do something about it. I’ll guide you thought this with simple words, no jargon, and no fluff. Ready?
1) What is central sensitization?
Think of your nervous system as a volume control for pain. Central sensitization is when that volume gets stuck on HIGH.
Your brain and spinal cord start making pain signals louder—even when nothing is actually hurting your body.
The result? You feel more pain, from more places, more often. Things that shouldn't hurt start to hurt. The pain becomes chronic and brings fatigue, brain fog, and other problems.
This is a real physical change in your nervous system.
| Type of Pain | What It Means | Example |
|---|---|---|
| Nociceptive | Tissue damage or inflammation | Arthritis, sprains, broken bones |
| Neuropathic | Nerve damage | Diabetic neuropathy, sciatica, shingles pain |
| Nociplastic (Central Sensitization) | Nervous system amplifying signals | Fibromyalgia, widespread chronic pain |
2) What does it feel like?
Here are the specific signs that your nervous system has become too sensitive:
When normal touch hurts
A gentle hug stings
Your bra or belt feels painful all day
Shower water feels too intense
Brushing your hair hurts
Getting a massage is painful instead of relaxing
Medical term: Allodynia (pain from things that shouldn't hurt)
When small injuries feel huge
You stub your toe lightly and the pain is extreme
A blood draw feels like stabbing
Someone bumps you and you hurt for hours
A paper cut feels like a major wound
Medical term: Hyperalgesia (bigger pain response than normal)
When pain spreads
You hurt your ankle, now your whole leg hurts
Back pain moves to your neck and shoulders
A headache on one side spreads to your whole head
Wrist pain spreads to your entire arm
Medical term: Spreading sensitization (the hyperexcitability can cause pain signals to spread beyond the original injury site.)
When pain won't go away
Your broken bone healed months ago, but still hurts
The infection is gone, but you still hurt
Your surgery was successful, but you're in pain
A strain that should heal in weeks has hurt for years
Medical term: Chronification (acute pain becoming chronic, even after tissue has healed)
Do You Have These Symptoms?
- Light touch causes pain (clothing, hugs, sheets)
- Small injuries feel much worse than they should
- Pain has spread beyond the original injury
- Pain continues long after healing
- Extreme fatigue that sleep doesn't fix
- Brain fog or trouble concentrating
- Sensitive to lights, sounds, or smells
- Sleep problems
- Feeling dizzy or unsteady
- Stomach or digestive problems
— 3 Key concepts to understand —
I) Pain vs. Suffering: They're Different
Pain = The physical feeling (throbbing, burning, aching)
Suffering = Everything else:
Canceling plans over and over
Fear it will never get better
Feeling alone because friends stopped calling
Money stress from medical bills
Not being able to play with your kids
Losing the life you used to have
When your nervous system is sensitized, your brain turns a pain level of 3 into an 8. Then it adds all that suffering on top.
Treatment needs to help both the pain AND the suffering.
😣 Pain
- Physical feeling
- Throbbing, burning, aching
- Can rate it 1-10
😔 Suffering
- Canceled plans
- Fear & worry
- Lost friendships
- Money stress
- Lost activities
- Grief for old life
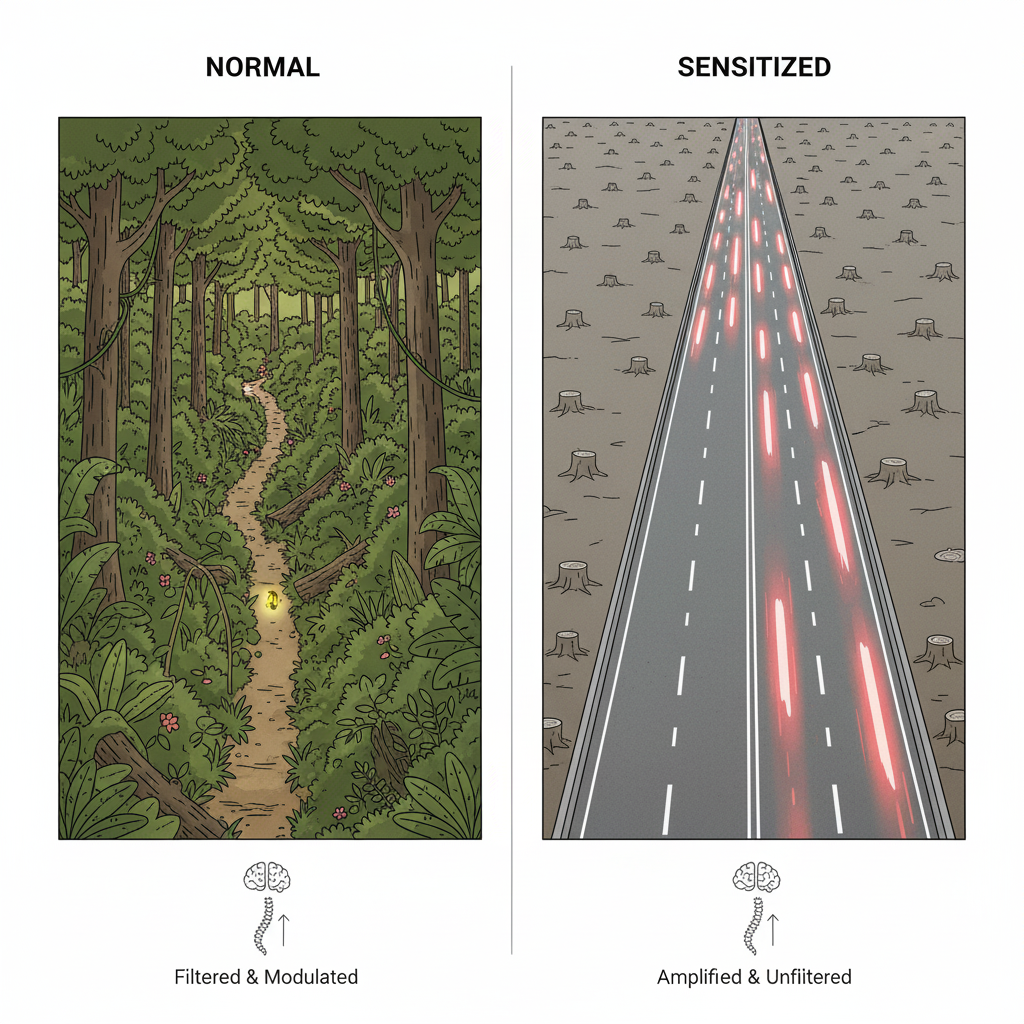
II) How Your Pain System Changes: The Highway Story
Here's how central sensitization develops (my favorite analogy to explain to my patients):
From Jungle to Highway : how the pain signal becomes amplified and dysregulated
Stage 1: The jungle path (normal)
Imagine a dense jungle between your spinal cord and brain. When you feel pain, a signal walks through the jungle on a narrow path.
The path is hard to walk. Trees and plants slow it down. By the time it reaches your brain, the signal has been filtered. Your brain gets the message: "Be careful, something hurts."
When you heal, the signals stop. The jungle path stays overgrown. This is normal.
Stage 2: Clearing the path (repeated pain)
Now imagine the pain signal walks that path every day, many times a day.
Each time it walks through, it clears away more plants. More signals follow. The path gets clearer.
The narrow path becomes a trail. Then a dirt road. Trees get cut down. Each trip makes the next trip easier.
Your nervous system is learning to send pain signals faster.
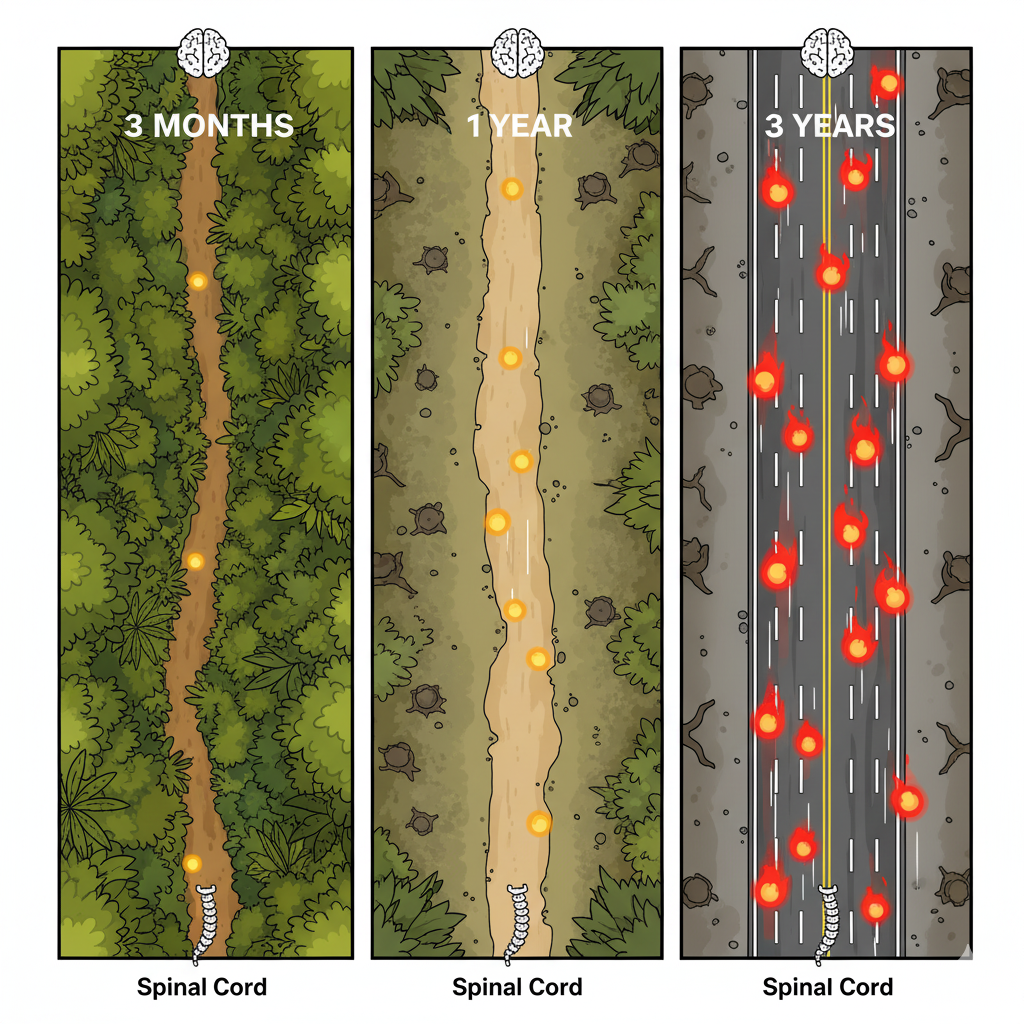
Important: The 3-6 month window
This change usually happens in 3 to 6 months.
In the first weeks or months after getting hurt, your pain makes sense. You're injured. Your body is healing.
But if the pain keeps going past 3-6 months, something changes. The pain transforms. Your original injury may have healed, but the pain pathway stays changed.
A doctor might say, "Your X-ray looks good. I don't know why you still hurt." They're not wrong about the healing. But the problem moved from your injury to your nervous system.
This is why getting help early matters. If you treat pain well in those first months, you might stop the nervous system from getting stuck.
If it's been years since your pain started—it can still be treated. But it helps to understand why the pain stayed even though you healed.
Stage 3: The superhighway (central sensitization)
After months or years, the narrow jungle path becomes a five-lane superhighway.
Signals race down a clear, wide road from your spinal cord to your brain. No plants blocking it. No filters. No brakes.
Here's the big problem: Once the highway is built, every signal uses it (because you don’t walk the small road in the forest where it’s hard and slow, when you can safely make it fast while driving on a highway!) .
Light touch? Uses the highway.
Gentle pressure? Uses the highway.
Temperature change? Uses the highway.
Normal body signals? Use the highway too.
Your brain gets all these signals and thinks: DANGER. PAIN. THREAT.
Your nervous system can't tell the difference between real danger and normal feelings anymore.
Why it stays changed
Once the highway is built, it stays built. In brain science: "Neurons that fire together, wire together."
Even after you heal, the highway is still there—ready to make any signal louder.
This is why you need treatment to:
Calm the nervous system (less traffic on the highway)
Build new pathways (retrain with pain-free movement)
Restore the brakes (strengthen your body's pain controls)
Good news: Your nervous system can change. You can build new pathways and quiet old ones. But it takes time and the right approach.
Your nervous system stays activated over time : the “pain highway”
III) When Doctors make it worse…
Sometimes the healthcare system makes pain worse. Here's how:
Words matter. Your brain's alarm system listens to your doctors.
When a doctor says:
"Your MRI looks really bad"
"This is serious"
"There's nothing we can do"
"This usually gets worse"
Your brain hears: DANGER!
And what happens? Your nervous system makes pain louder.
—> Ways healthcare can hurt
Dismissive words: "It's all in your head," "You're just stressed," "Your tests are normal so nothing is wrong"
These words are harmful. They make you feel worse, delay real help, and increase pain.
Scary reports: Medical reports listing "degeneration," "bulging discs," "arthritis"—these findings are common and often not the source of pain. But reading them makes you scared, and fear makes pain worse.
Too many procedures: Multiple surgeries that don't fix the real problem can make you think something is broken—keeping your alarm system on.
Wrong medications: Prescribing opioids for central sensitization makes it worse, not better.
—> What smart doctors do instead:
Doctors who understand key concepts of central sensitization will say:
"Your pain is real, and we will help, even if it might not be perfect"
"These findings are common and don't predict your pain"
"Your nervous system is sensitized—we can treat that, let’s talk about our options"
"Let's focus on what you can do, your function is key in you quality of life"
3) What causes central sensitization?
> Main triggers
Long-lasting pain or inflammation: Pain that goes on and on slowly changes your nervous system.
Nerve damage: Damaged nerves (from diabetes, infections, shingles) send confused signals. Your nervous system can't understand them and overreacts.
Brain or spinal cord injury: Strokes, trauma, or diseases can change how your brain handles pain.
> Things that make it worse
Constant stress: Your brain handles physical and emotional stress the same way. Stress keeps your nervous system on high alert.
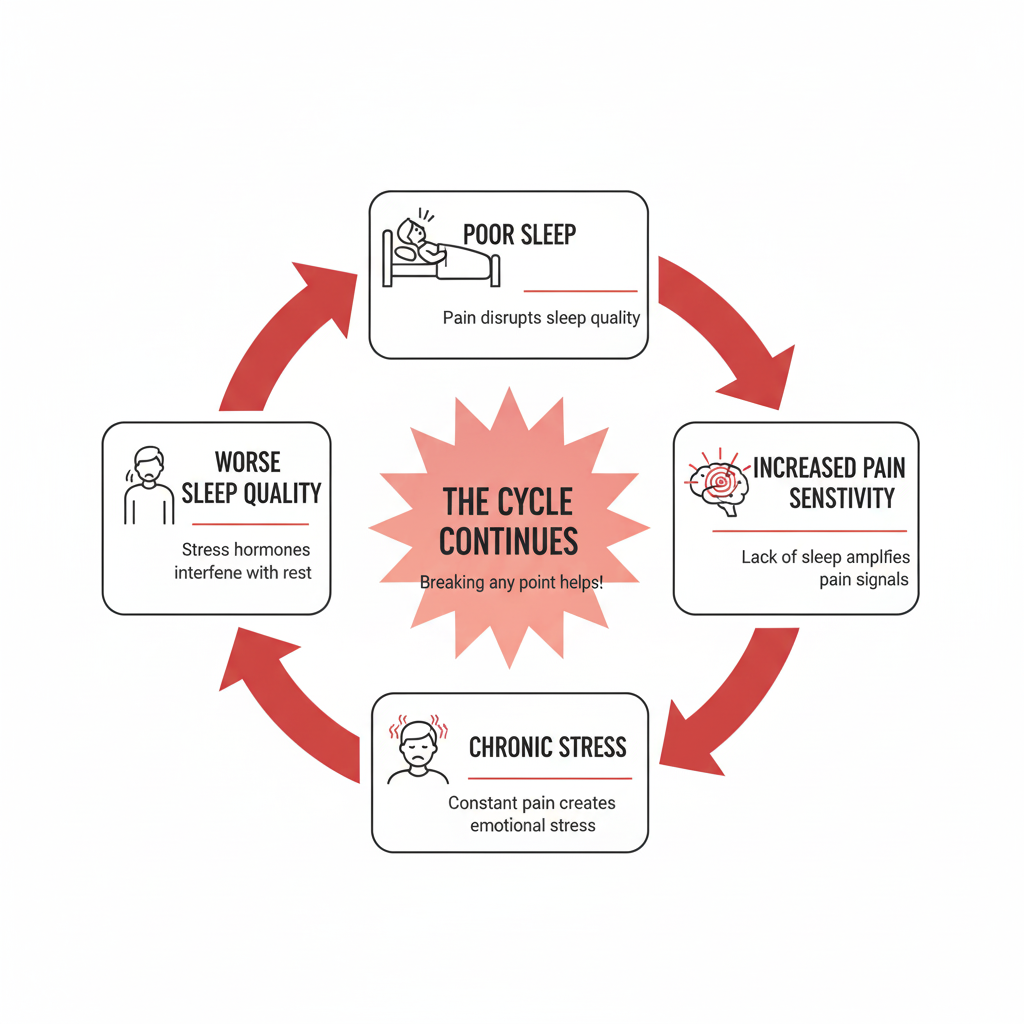
Bad sleep: Pain stops you from sleeping. Poor sleep makes pain worse. It's a cycle.
Negative thoughts: Thinking "This will never get better" or "Something is terribly wrong" makes pain pathways stronger. Your brain treats fear as a threat.
Being alone: Avoiding friends and activities makes pain worse. When you're alone, you have nothing to distract you, and depression grows.
Family history: Central sensitization runs in families. Some people's nervous systems are more likely to get stuck this way.
> Conditions linked to central sensitization:
| Body Area | Common Conditions |
|---|---|
| Muscles & Joints | Fibromyalgia, chronic back/neck pain, arthritis, TMJ, complex regional pain syndrome |
| Headaches | Migraines, tension headaches |
| Belly & Pelvis | Irritable bowel syndrome (IBS), painful bladder, chronic pelvic pain, painful periods, vulvodynia |
| Nervous System | Multiple sclerosis, post-stroke pain, central pain syndrome |
4) Treatment: retraining your nervous system
There's no quick cure. But your nervous system CAN be retrained. You need to work on multiple things at once.
1. Movement: The 10% rule
Why it works: Exercise helps your brain make natural pain relievers. It slowly teaches your nervous system that movement is safe.
Most people do this wrong:
You feel good one day, so you do EVERYTHING. You clean, walk, do errands, garden. By night, you're in terrible pain. The flare lasts weeks. You think, "Exercise makes it worse."
The right way:
Think of training for a marathon (I’m not telling you to train for a marathon). You don't just wake up and run 26 miles. You build slowly.
The 10% rule: Start with what you can do now—even 5 minutes. Then add only 10% every two weeks. Even if it feels good, limit yourself! This is the KEY.
Which means for example:
Week 1-2: Walk 10 minutes daily
Week 3-4: Walk 11 minutes daily
Week 5-6: Walk 12 minutes daily
It feels slow. But it works because you retrain your nervous system without setting off the alarm. After 6 months, you might be able to walk 25-30 min easy, without flaring up.
Tips:
Pick something you enjoy (swimming, dancing, cycling)
Start small—even 2 minutes counts at first.
Do it every day rather than once a week for a long time
Mix it up: walking, stretching, strengthening
Build up resistance and endurance
2. Sleep
Bad sleep makes pain worse. Good sleep gives your nervous system a chance to calm down.
Sleep is always one of my priorities when first building a plan with a patient. They need to sleep! (I would say almost “whatever it takes”)
What helps:
Go to bed and wake up at the same time every day. Avoid eating before bed.
Make your bedroom dark, cool, and quiet
No screens before bed. Listen to a sleep meditation or a audiobook instead.
Get help if you have sleep apnea (this is a major one +++)
Talk to your doctor if you need more help.
3. Food
Why: Your brain needs the right fuel to make chemicals that control pain and mood. Think “anti-inflammatory”. Here are simple principles when you are doing you groceries:
Buy real food (not processed)
Make meals with foods that fight inflammation (fruits, vegetables, fish)
Make sure you get enough protein for muscle mass
Limit sugar and junk food
Eat what you cook at home. Enjoy dinner at the table while talking to your family.
4. Calm your stress
Why: Stress makes pain louder. A thousand times.
What works:
Meditation or mindfulness
Deep breathing
(chair) yoga, tai chi or Qi gong can help as low impact (free youtube videos!)
Time outside, in nature is the best.
Hobbies you enjoy
Hug someone, including your pet if you have one. It release oxytocin.
5. Talk therapy
Cognitive behavioral therapy (CBT): Helps you change thoughts that make pain worse. Research shows it really works.
Mindfulness: Teaches you to notice pain without fighting it. This can help you suffer less even if you still feel pain.
Physical therapy: A good PT creates a plan to help you move more without causing flares.
6. Stay connected
Remember : Being alone makes pain worse.
When you avoid people:
Nothing distracts your brain from pain
You lose support that helps you feel better
You get depressed, which makes pain louder
What helps:
Join a chronic pain support group
Keep at least one friend close
Ask family for specific help
Tell people your limits without saying sorry
Talk about things other than pain sometimes
[TABLE 4: Treatment Toolbox]
7. Medications
Medicine can help but works best with the other treatments above.
What helps:
Anticonvulsants (gabapentin, pregabalin): Calm overactive nerves
Antidepressants (duloxetine, amitriptyline): Work on brain chemicals that affect pain and mood
Ketamine: For ++ severe cases only (harder to get, more risks.)
CRITICAL: Avoid Opioids
Strong research shows opioids make central sensitization worse, not better.
They cause "opioid-induced hyperalgesia" — they actually increase pain.
If you're taking opioids now, talk to your doctor about slowly and safely stopping them.
If you're taking opioids now, talk to your doctor about slowly stopping them safely.
Note: Regular pain pills like ibuprofen don't help the central part of pain.
8. Other helpful tools
These can help along with the main treatments:
TENS units: Small electric pulses that change pain signals
Heat or cold: Try both to see what helps
Acupuncture: Some research supports it
Massage: Good for tight muscles (find someone who knows chronic pain)
Creams: Capsaicin, lidocaine patches
Magnesium: May help muscles relax and sleep improve
Your Treatment Toolbox
Movement
Start small, build slow using the 10% rule
Sleep
Regular schedule and good sleep habits
Nutrition
Real food that fights inflammation
Stress Control
Meditation, breathing, yoga, nature
Therapy
CBT, mindfulness, physical therapy
Social Support
Stay connected with people who care
Right Medications
Central-acting drugs (NOT opioids)
Extra Tools
TENS, heat/cold, massage, acupuncture
How to talk to your Doctor.
Before your visit:
Write down your pain for 1-2 weeks (when it hurts, what makes it better/worse, where it is). Think about which type of pain you have. Write your questions down before the visit.
At your visit:
Be specific: Instead of "Everything hurts," say: "I have pain that spread beyond my original injury. Even light touch hurts now."
Say the key signs:
Pain that won't go away after healing. Pain from light touch. Bigger pain response than normal. Pain that spreads. Fatigue, brain fog, sensitivity to light/sound.
Use the words: "I read about central sensitization and nociplastic pain. My symptoms match. Could this be what I have?"
Ask: "If this is central sensitization, what treatments work? Should I see a pain specialist?"
If your doctor dismisses you:
Ask to see a pain specialist. Get a second opinion. Look for pain clinics in your area
If you have more than one type of pain:
Say: "I think I have arthritis pain AND central sensitization making it worse. Can we treat both?"
This matters because different types need different treatments.
Conclusion
Your pain is real, even if not visible.
Central sensitization is a real change in your nervous system. The highway from your spinal cord to your brain is real. The changes in your brain cells are real.
For too long, people with this condition have been told it's not real or it's just stress. If that happened to you, you deserved better from the healthcare system.
What matters is that central sensitization can be treated. Not fast, not easy, but truly treated. Your nervous system learned to make pain louder. It can learn to quiet down.
You need:
Movement that slowly rebuilds strength
Sleep that lets your nervous system rest
Food that fights inflammation
Ways to calm stress
People who support you
Therapy that helps your thoughts
The right medications
You'll have good days and bad days. That's normal. But understanding what's happening helps you know you're on the right path.
You have a diagnosis. You know how it works. You have treatments.
The jungle became a highway. Now we build new paths, restore the brakes, and teach your nervous system it's safe to turn down the volume.
References
Woolf CJ. Central sensitization: Implications for the diagnosis and treatment of pain. Pain. 2011;152(3 Suppl):S2-S15. doi:10.1016/j.pain.2010.09.030
The foundational paper defining central sensitization
Albrecht DS, Forsberg A, Sandström A, et al. Brain glial activation in fibromyalgia - A multi-site positron emission tomography investigation. Brain Behav Immun. 2019;75:72-83. doi:10.1016/j.bbi.2018.09.018
Breakthrough PET scan study showing visible brain inflammation in fibromyalgia patients
Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology. 2018;129(2):343-366. doi:10.1097/ALN.0000000000002130
Comprehensive review of neuroinflammation's role in central sensitization
Lee M, Silverman SM, Hansen H, Patel VB, Manchikanti L. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. 2011;14(2):145-161.
Evidence that opioids worsen central sensitization
Clauw DJ. Fibromyalgia: A clinical review. JAMA. 2014;311(15):1547-1555. doi:10.1001/jama.2014.3266
High-impact clinical review of fibromyalgia and central sensitivity
Kosek E, Cohen M, Baron R, et al. Do we need a third mechanistic descriptor for chronic pain states? Pain. 2016;157(7):1382-1386. doi:10.1097/j.pain.0000000000000507
Introduction of "nociplastic pain" terminology
Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: An overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4(4):CD011279. doi:10.1002/14651858.CD011279.pub3
Evidence for exercise in treating chronic pain
Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11:CD007407. doi:10.1002/14651858.CD007407.pub3
Evidence for CBT and psychological approaches
Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: A systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162-173. doi:10.1016/S1474-4422(14)70251-0
Comprehensive medication evidence from high-impact journal
Moseley GL, Butler DS. Fifteen years of explaining pain: The past, present, and future. J Pain. 2015;16(9):807-813. doi:10.1016/j.jpain.2015.05.005
Pain education and neuroscience education approaches
Notes on References
These references represent current evidence-based understanding of central sensitization, chronic pain mechanisms, and multimodal treatment approaches. The field continues to evolve, and readers are encouraged to consult with healthcare providers for personalized medical advice.
Conflict of Interest Statement: The author has no conflicts of interest to declare related to this article.
Last Updated: November 2025